Obesity constitutes a major global health burden
According to the World Obesity Federation, the worldwide prevalence of obesity has more than tripled between 1975 and 2022. Both adults and children are impacted.
In 2022, over 1 billion people (about 880 million adults + 159 million children/adolescents) were estimated to be living with obesity.
The global adult population with obesity is projected to increase from ~524 million in 2010 to ~1.13 billion by 2030 (+115 %).
Compared with people of healthy weight, those with overweight or obesity are at greater risk for many diseases, including diabetes, high blood pressure, cardiovascular disease, stroke, and at least 13 types of cancer, as well as having an elevated risk of death from all causes.
Impact of obesity on cancer development
There is a strong and well-established relationship between obesity and cancer. Obesity increases the risk, recurrence, and mortality of several types of cancer.
A working group from the International Agency for Research on Cancer (IARC) reviewed over 1,000 studies and found consistent evidence that higher levels of body fat are linked to an increased risk of several types of cancer.
About 4–8% of all cancers are attributed to obesity. Obesity is a risk factor for several major cancers, including post-menopausal breast, colorectal, endometrial, kidney, esophageal, pancreatic, liver, and gallbladder cancer. Excess body fat results in an approximately 17% increased risk of cancer-specific mortality.
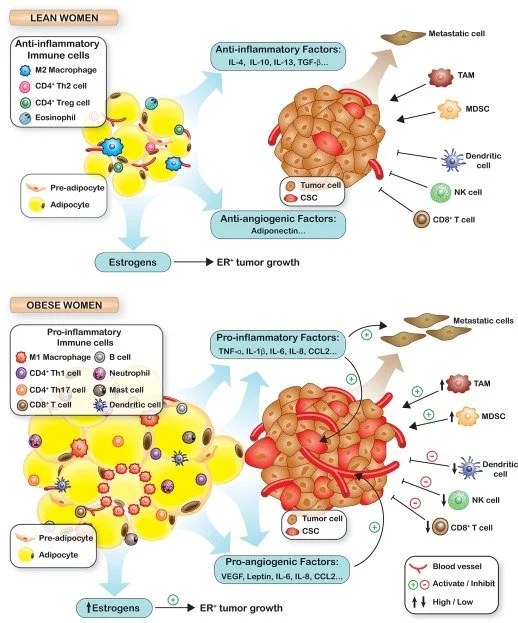
Obesity creates an internal environment — with excess hormones, inflammation, immune disruption, and altered cell signalling — that supports the initiation, growth, and survival of cancer cells.
For example, during the expansion of obese adipose tissue, preadipocyte differentiation is impaired, and hypoxia activates hypoxia-inducible factor 1 (HIF-1), leading to a decrease in adiponectin expression and an increase in leptin. HIF-1 promotes angiogenesis by inducing the expression of vascular endothelial growth factor (VEGF), which is known to have a direct impact on breast cancer invasion and migration.
Efficacy of existing therapies for obesity-related solid cancer
Existing solid cancer drugs may be less effective in obese patients, as this population is often underrepresented in clinical trials, and there are limited data on optimal dosing and treatment response.
Many cancer drugs are dosed based on body surface area or weight. If trials include few obese patients, optimal dosing for this group may not be well-established, potentially leading to under- or over-dosing.
Obesity can change how drugs are absorbed, distributed, metabolised, and cleared from the body. Drugs tested mainly in non-obese populations may behave differently in obese patients.
Obesity alters hormone levels, inflammation, and immune system function, all of which can affect how cancer grows and responds to therapy.
Because obese individuals are often excluded or underrepresented in trials due to potential existing comorbidities, there is limited data on drug efficacy and safety for this group, making it uncertain whether standard therapies work equally well.
Our science
At SARKKOS Therapeutics, our research work is based on the principle that obesity goes beyond being merely a risk factor; it serves as a molecular driver of cancer.
Thus, SARKKOS Therapeutics is developing a pipeline of small-molecule inhibitors that directly target a specific cell receptor, which we believe plays a role in modulating obesity-linked oncogenic pathways in solid tumours.
We aim to build first-in-class therapies that intercept cancer at its metabolic roots, offering new hope for patients with obesity-associated solid tumours.
SARKKOS Therapeutics is advancing tailored therapies for individuals affected by obesity-related cancers.
Changes in Adipose Tissue During Weight Gain
Picon-Ruiz et al. Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention. CA CANCER J CLIN 2017;67:378–397
The Role of Obesity in Tumorigenesis
Picon-Ruiz et al. Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention. CA CANCER J CLIN 2017;67:378–397